Key Achievements
In 2019-20, the Clinical Excellence Commission:
- responded to the COVID-19 pandemic with rapid development and publication of 55 new clinical guidance documents on infection control and prevention which attracted over 200,000 web site downloads
- supported the state-wide response to COVID-19 with development of resources for external agencies including aged care facilities, private hospitals, the NSW Police Force and Transport NSW
- as part of the primary function to minimise potential harm, issued 17 safety alert broadcasts, distributed 12 medication safety communications and 13 medication safety updates
- in response to 800 notifications, conducted risk assessments on medical devices, medicines and biological agents with nine identified as high risk, requiring system level response led by the newly established Critical Response Unit
- delivered clinical data to more than 29,000 local users in NSW Health through the CEC’s Quality Improvement Data System enabling over 800 improvement projects and generating 15,000 monthly reports
- educated 63 NSW Health staff in improvement science through the Executive Clinical Leadership Program and 249 graduates in Foundational Clinical Leadership Program through the CEC’s Quality Improvement Academy
- assisted preparations for commencement of legislative changes for serious incident management, including transition to use of the online ims+ platform including development of a Preliminary Risk Assessment and alternate investigation methodologies to Root Cause Analysis
- under the Mental Health Patient Safety Program, delivered quality improvement training for 83 medical and clinical leads and trained 51 improvement coaches to support 73 frontline mental health teams in safety and quality improvement projects
- delivered weekly personal protective equipment (PPE) audits for Local Health Districts and Specialty Health Networks to assist identify potential issues with PPE supply
- conducted 226 clinical product assessments of personal protective equipment in collaboration with HealthShare NSW
- launched the Safer Baby Program in NSW aiming to reduce stillbirths by 20% by 2023.
Connecting with Aboriginal Consumers

REACH out for safety

Take Own Leave Report
As an extension of the REACH program , the CEC partnered with the Aboriginal REACH Advisory Group to develop an information flyer for Aboriginal patients, families and carers to encourage escalation of concerns about patient deterioration.
The Advisory Group consulted with Aboriginal Elders, community members and healthcare staff in metropolitan and regional areas.
In partnership with the NSW Centre for Aboriginal Health, the CEC released the Diagnostic Report: Understanding contributing factors for Take Own Leave in NSW health organisations.
The report explored four levels of interdependent levels of responsibility – system, organisation, community and individual – and identified ten key themes for consideration to reduce harm and improve care of Aboriginal people in hospitals across New South Wales. A key finding related to the importance of building cultural safety for Aboriginal consumers through cultural awareness and cultural sensitivity.
The artwork featured in both documents is 'Health Custodian' by Jasmine Sarin, commissioned by the CEC.
QIDS and QARS
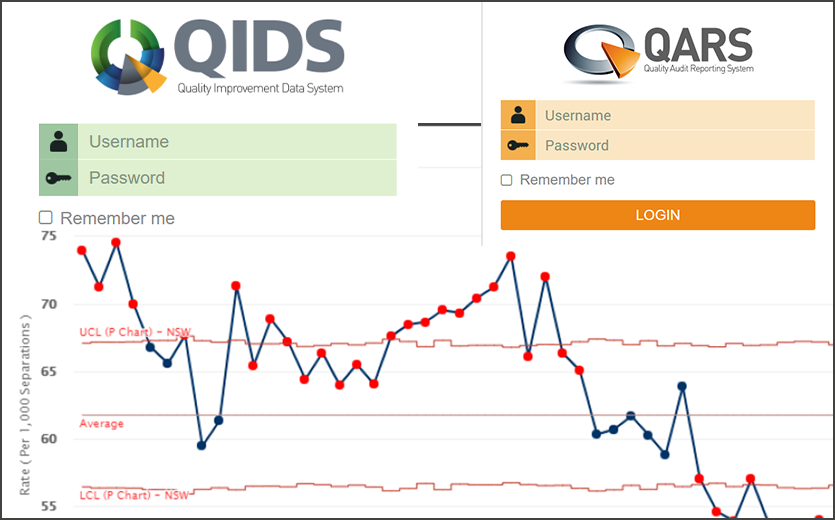
QIDS
The CEC-developed Quality Improvement Data System (QIDS) provides users at all levels of an organisation with a single point of access to information and tools for the purpose of improving the quality and safety of health service delivery. QIDS transforms data from several sources into a unified platform with standardised and customisable analytic and improvement tools. It enables users to translate raw data into insights such as current outcomes, trends over time, unwanted clinical variation, harm and outcome measures of improvement innovations.
Growth in the use of CEC’s QIDS continued its steep rise in 2019-20 as clinicians discovered the value of using local data to drive local quality improvement projects. At the end of the reporting year QIDS had 29,000 users – an increase of 500% year on year. These users had created more than 800 improvement projects with around 15,000 reports generated every month.
QIDS also continued to develop in capacity and capability adding a Morbidity and Mortality Meeting module to provide a secure platform for clinical teams. In anticipation of the improved source of data from ims+, the CEC worked with eHealth to facilitate reporting of incident data through the QIDS application. Enhancements to QIDS include the availability of data from emergency departments.
The CEC continues to provide education and training opportunities for clinicans and clinical teams across NSW Health. In 2019, Dr James Mackie and Dr Jun Bai embarked on a series of roadshows throughout NSW to introduce the QIDS platform to clinicians and senior managers. The roadshow’ s main focus was to highlight the value of QIDS as a platform for processing data and sharing information with a focus on patient safety and quality improvement activities.
QARS
Quality Audit Reporting System (QARS) is an electronic tool developed by the CEC to help to improve the quality and safety of health care provided by local health districts, speciality health networks, pillars and NSW health service providers (the Health Entities). The QARS application has three modules including Audit, Survey and ReACT.
In 2019-20, the data and analytics team completed major upgrade to the QARS system. The upgrade will enhance functionality and security. The major new addition is the QARS REACT module to improve the management of product recalls and other high priority information requiring immediate action at facilities across NSW.
Meeting the COVID-19 Challenge

At the end of 2019, with news of an outbreak of a highly infectious novel coronavirus in China, preparations were begun for potential impact on the NSW Health system. From November, the Clinical Excellence Commission’s (CEC) Healthcare Associated Infections team began building an understanding of the nature of the new coronavirus and challenges for infection control.
While NSW Health led the state response, on declaration of a pandemic on 11 March 2020, the CEC had a specific role under the NSW Influenza Pandemic Plan. This included providing infection prevention and control and patient safety advice and expertise to the Ministry of Health and developing state-wide strategies and resources to maintain high levels of compliance with infection prevention and control and patient safety recommendations.
An expanded COVID-19 Infection Prevention and Control (IPC) Response Team was formed in late March with many of the CEC’s internal workforce redeployed in support roles. Seven specialist CEC staff were also re-deployed, on request, to assist the Ministry of Health COVID-19 or clinical teams in Local Health Districts.
By April 2020, two more specialists joined the IPC Response team to meet increasing requests from clinicians and the community for guidance on infection control. The expanded team continued to demonstrate outstanding commitment, responding to requests at all levels of care. Advice was also provided to the private aged care sector, in particular; Newmarch House; Dorothy Henderson Lodge and Bodington nursing care homes.
During this time, the CEC ensured weekly medication safety notices and infection control guidelines were shared across the NSW Health system.
CEC representatives were present on all 30 of the newly created Communities of Practice (CoPs) and leading the CoP for Infection Prevention and Control and Infectious Diseases. Twenty-five percent of state-wide CoP issues were escalated to the CEC. Themes from CoPs included use of Personal Protective Equipment (PPE) in various clinical high-risk settings; reuse and extended use of PPE and home visits guidance for community workers caring for COVID-19 patients.
From February 2020 to June 2020, expert advice on supply, provision and correct use of Personal Protective Equipment emerged as a critical factor in limiting infection in clinical and other settings where services required close contact. To deal with the influx of commercial products offered to the health system, a new collaboration was formed between experts in infection control and procurement experts from internal corporate services agency, HealthShare NSW. Over five months, the team assessed over 226 PPE clinical products.
Videos on correct use of PPE were developed and produced by the CEC resulting in 35,000 online views. In addition to the CEC’s publicly available resources, collaboration with non-health agencies included assistance to: Transport NSW, Fire and Rescue NSW, NSW Education, the NSW retail industry, NSW Courts and the NSW Police Force.
Alongside meeting demands over this intense response period to the acute pandemic, the CEC continued to deliver its responsibilities as the lead agency for safety and quality in NSW.
The CEC went on to deliver an intense and sustained effort to support and protect the NSW Health community and, beyond Health, to other essential services personnel.

Kathy Dempsey
As Senior Manager of the Healthcare Associated Infections team, Kathy Dempsey demonstrated commitment, energy and leadership in the fight against COVID-19 in NSW, inspiring and motivating her colleagues in the CEC and the wider Health community. While under considerable pressure, Kathy continued to influence the system to meet clinical guidelines and exacting standards on infection prevention and control in the provision of safe patient care at the same time protecting health workers in this challenging time.
Kathy led her expanded team as well as the CEC’s agency response and provided individual expertise in infection control across a wide range of state, interstate and federal committees and consultations including as clinical lead for the NSW Health Infection Prevention and Control Community of Practice and a member of the NSW Clinical Council.
The CEC’s COVID-19 team provided consistent and timely responses to requests for advice and expertise at all levels of care, developing and updating existing resources on Personal Protective Equipment (PPE) to support and meet demand from frontline teams. Kathy was also involved in collaboration with Ministry of Health leaders and other organisations such as HealthShare NSW on assessment of a high volume of PPE products. She provided expert infection control and prevention advice to the private aged care sector as needs emerged and participated in the Royal Commission into Aged Care.
Kathy is the NSW state representative of the National Infection Control Expert Group (ICEG) and a board member for the Australasian College for Infection Prevention and Control (ACIPC). She is widely considered a leader in the field of Infection Prevention and Control across the state and nation.
Our thanks
In the preparation of this document we would like to thank management, clinical staff and communications teams in the following local health districts: Illawarra Shoalhaven, Mid North Coast, Murrumbidgee, Northern Sydney, Western NSW and Western Sydney.







